The transnational Sana Young Professional network brings together young professionals from hospitals, industry and Sana to discuss current challenges in the healthcare market. A special group of young members of the purchasing community has been working intensively on the topic of digitalization. Here is her summarized contribution on the topic:
From cheese and chocolate to digital patient files? Can Germany learn something from Switzerland here too?
Swiss idyll, quiet locations and fantastic mountain scenery.
Not only since the Ricola advertisement have many Germans perceived Switzerland as an island of bliss in the middle of Europe. During the Covid-19 pandemic, the Swiss had the courage to return to normal life more quickly. In general, structures in the healthcare sector appear to be more agile, more digitalized and faster to implement than in highly bureaucratized Germany[1]. One example of this – if first impressions are to be believed – is the digital patient file, which the Germans are barking up the wrong tree about. But what do the Swiss do differently or better than the Germans? Let’s take a look at the digital patient file as an example.
Before that, let’s clarify: What is the digital patient record anyway? To achieve this, we would like to start one step earlier with the patient pathway:

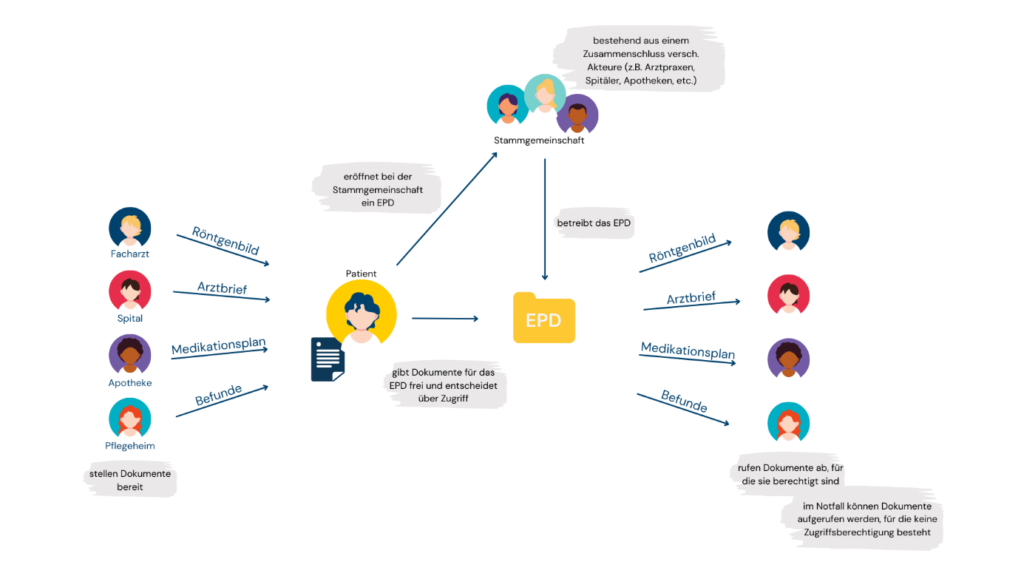
[2]
A medical history is always highly individual. In order to speak of the “same” here, we will make life a little easier for ourselves at this point and show a path from the occurrence of the problem to rehab. So where does the patient pathway begin? Each
according to the nature of the emergency at the family doctor or in the emergency room. We don’t assume the worst – that’s why we let our patient “Pauli” go to the GP with a twinge in his chest and pain in his left arm. As his overall condition is critical, the doctor refers him directly to the hospital around the corner. Pauli finds his way to the hospital via the emergency room and, after the examinations, directly to the cardiac catheterization measuring station: heart attack! Nowadays, fortunately, he can be treated with stents and after a few days on the ward, he goes home for a short break before Pauli goes into rehabilitation for six weeks so that his heart can recover a little through targeted exercises.
We now have many parties involved in this process: the referring doctor, staff in the emergency room, the health insurance company, attending doctors in the hospital, the family doctor and finally the staff in the rehabilitation facility. At best, they should all pass on the right information to the right recipient at the right time – digitized these days, of course. After all, I can track my postal parcel almost anywhere in the world in real time. The patients too? This approach is being pursued with the digital patient file and is intended to serve as a central element of networked healthcare[3].
Now let’s take a look at how Switzerland and Germany compare when it comes to patient records:
Switzerland.
The digital patient record (EPR) has been gradually introduced since 2020. Estonia has been using the digital patient file since 2008[4].
The aim of the EPD is to facilitate the exchange of information between all parties involved. So far, Swiss patients have had sovereignty over their data. Specifically, he can decide for himself which data is uploaded. It all sounds quite good, but even in liberal Switzerland there are one or two hurdles to overcome: Organizationally, hospitals must be members of parent associations that offer EPDs. This can lead to regional differences – one parent association serves the canton of Zug, the next serves all cantons – which means that the EPR is not yet in use across the board. As always, the issue of money also plays a role: although the EPD was subsidized with CHF 30 million, sustainable financing is not guaranteed. In addition, participation in the EPD is voluntary for doctors, pharmacists and physiotherapists in private practice before 2022[4]. So if our patient Pauli lives in Switzerland, he needs to find out in advance about the local conditions in order to actually benefit from the EPD.
What is the situation in Germany?
Slightly later than Switzerland, Germans have been able to obtain a digital patient file (ePA) from their health insurance provider since January 1, 2021. Thanks to the General Data Protection Regulation (GDPR), all patients in Germany can also have a say in the content of their digital patient file. In typical German fashion, a few bureaucratic hurdles are built in: In the first stage, only the patient himself could add data to his file. Doctors can only read the ePA with an individual connector – which of course costs money. Since 2023, an authorization concept has also been in place, which releases or does not release data according to individual decisions. So if our heart attack Pauli is German, he must have made sure himself that he has a patient file and that it is filled with information. It therefore seems unsurprising that less than one percent of people with statutory health insurance still use the digital service. This is to be remedied by the so-called opt-out principle, whereby an electronic patient file is to be automatically available to all people with statutory health insurance from the end of 2024. Patient Pauli must therefore object to the creation of an e-file in future. Innovative? Far from it: Austria has been practicing the opt-out principle since its introduction in 2016.
Conclusion.
Overall, both systems – in Switzerland as well as in Germany – have not really reached patients, let alone finally matured. The application varies, the added value is not recognizable across the board and the system is complex. As is so often the case, knowledge is power. In both countries, I can decide for myself what I, as a responsible patient, release via the patient file.
There are still a few hurdles to overcome in both countries.
Sources:
[1] https://www.laenderdaten.info/laendervergleich.php?country1=CHE&country2=DEU, as at 26.05.2023
[2] https://www.flaticon.com/free-icons/rehabilitation” title=”rehabilitation icons”>Rehabilitation icons created by Flat Icons, as of 22.06.2023; https://www.flaticon.com/free-icons/patient” title=”patient icons”>Patient icons created by Freepik, as of 22.06.2023; https://www.flaticon.com/free-icons/muscle-pain” title=”muscle pain icons”>Muscle pain icons created by AomAm, 22.06.2023
[3] https://www.bundesaerztekammer.de/themen/aerzte/digitalisierung/digitale-anwendungen/telematikinfrastruktur/epa, as at 26.05.2023
[4] http://www.informatik.uni-oldenburg.de/~iug13/pa/index.php/vergleich-mit-anderen-laendern.html, as at 26.05.2023
[5] Dissemination of the EPR – eHealth Suisse (e-health-suisse.ch), as at 15.06.2023